Images shown are not intended to be used for the diagnosis or treatment of a disease or condition.
Is your dermatology practice ready for digital pathology? Most physicians feel the need to create a more efficient patient care process, but many don’t realize the far-reaching advantages of using a digital pathology workflow.
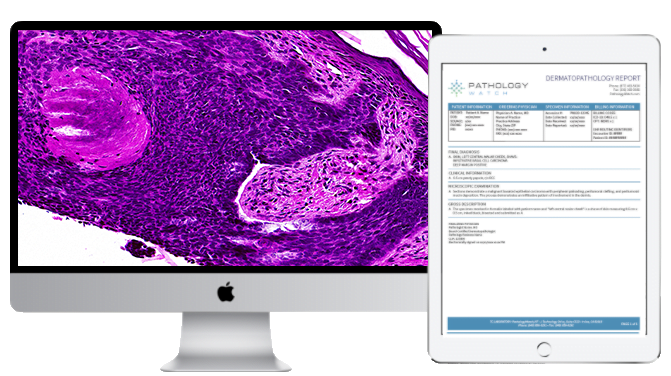
According to a 2018 survey of US healthcare consumers and physicians, up to 69 percent of physicians, including dermatologists, are interested in increasing the use of digital tools to improve patient care, among other purposes. Due to recent advances in digital pathology, there is an alternative for dermatology clinics that typically rely on microscopy and glass slides: the online access of digital slides and reads from academic-level dermatopathologists. Companies like PathologyWatch, which offers whole-slide imaging to dermatologists, are helping digital pathology quicken its pace to the forefront of dermatology patient care.
As complications like COVID-19 force healthcare providers to consider alternative options to traditional office visits, dermatologists must find a way to abide by HIPAA guidelines while remaining profitable. Experts agree that a digital system can be cost neutral and even save money for medical practices.
Three critical factors contribute to a successful dermatology practice: efficiency, accessibility, and customer satisfaction. Each of these can improve with the adoption of a digital pathology platform.
1. Digital pathology is the solution for a more efficient and profitable pathology process.
According to experts, current trends in the traditional pathology model were already facing transformation. Based on data collected by DARK Daily, between 2007 and 2017, the pathologist workforce reduced its numbers by almost 18 percent, while the pathologist’s diagnostic workload rose by 41.7 percent.
Such imbalance is a formula for potential disaster as technicians scramble to meet lab work demands while using manual processes to prepare slides, mail specimens, collect and organize test results, and input data for each patient’s specimen slide.
Those who work in labs recognize that a digital pathology system may help to reduce errors and create efficiency, even while the workload increases. Fortunately, adopting a digital workflow and imaging system reduces the risk of mistakes while inputting data, eliminates redundancy in handling slides, and speeds up the process for issuing test results. Laboratories that provide digital images of the glass slides can also result in 24/7 access to slides by clinicians.
2. Digitized slides enable collaboration among specialists.
With whole-slide images digitally cataloged, doctors can easily access a patient’s specimen themselves and securely share it anywhere and anytime with fellow pathologists. Such collaborative practices heighten the quality of care at all participating facilities rather than limiting expertise to one or two locations. “We place a lot of value in consulting, case sharing, and communicating in our practice so that each hospital receives the benefit of our combined knowledge and experience,” says Nicolas G. Cacciabeve, MD, a managing member at Advanced Pathology Associates.
Cacciabeve adds that incorporating whole-slide imaging into their practice workflow has led to an improvement in the way they do things. “It drives efficiency and improves access to expertise,” he says.
The ability to extend patient care to those who often face challenges accessing specialized care is an exciting feature of digital technology. For healthcare professionals, providing treatment to the most vulnerable communities, particularly those in rural communities, is a constant challenge.
According to the Office of Disease Prevention and Health Promotion, almost 25 percent of Americans living in rural areas do not have a primary care provider (PCP) or health center where they can receive regular medical services. And with skin cancer ranking as the most common form of cancer in the US, people living in rural, agricultural areas could particularly benefit from access to dermatopathologists, who can examine a digitalized specimen and work with a local physician to design a treatment plan. Such services wouldn’t be possible without digital pathology technology.
3. Improve customer confidence with a digital platform.
The expanded access and collaboration available with the adoption of digital pathology also results in equivalent or improved patient outcomes. Zoltan Laszik, MD, PhD, professor of clinical pathology at the University of California San Francisco School of Medicine, directed a team to collect results between 30 pathologists and 800 test slides distributed among three hospitals. “There was not a single case that was misdiagnosed because of the digital technology, and the benefits were immediate from hospital to hospital,” Laszik says. By improving access to expertise and facilitating collaboration, Laszik and Cacciabeve see digital pathology as a vehicle to increase the speed and accuracy of diagnosis while innovating the modern standard of patient care.
While digital technology isn’t new, the possibilities digital pathology creates for the dermatopathology field to streamline lab processes, expand patient access to specialized care, and improve customer satisfaction are exciting and work together to ultimately help physicians take better care of their patients.