Jan 27, 2022 | Dermatology Practice
By Eva Vertes George, MD
If you’ve toyed with the idea of starting your own dermatology clinic, you are not alone. In an industry worth almost $8.5 trillion with marked growth exceeding $800 billion by 2021, approximately 31.4 percent of physicians are independent practice owners.
Innovations in healthcare technology will likely trigger a new batch of medical startups utilizing emerging digital technologies to fill the growing need for dermatological care. The problem is that physicians have spent the majority of their time learning how to serve patients as dermatologists, not how to run businesses. That lack of business savvy may prevent many talented healthcare professionals from going into business for themselves.
Experts estimate over 5,000 dermatology businesses operate in the US, with indicators showing a consistent 1 percent growth in the dermatology industry since 2020. Cost, culture, and the customer determine whether a new practice is dialed in for future success as a solo practice or as part of a group practice.
Based on these factors, let’s discuss the advantages of (and a few of the possible deterrents to) joining an existing dermatology group practice based on cost, culture, and the targeted customer base.
Cost
Estimating the total cost to open and maintain a new clinic is likely the biggest obstacle for dermatologists planning to take the next step toward ownership. When you consider overhead costs associated with property, lab equipment, staff, marketing, and billing software, it’s no wonder that new clinic owners often underestimate the amount of money it takes to keep the doors open.
Because it often takes at least two years to turn a profit, Jerome Obed, DO of Broward Dermatology and Cosmetic Specialists in Florida, recommends having at least two years’ worth of money to live on when first opening a private dermatology practice.
If cash flow isn’t reliable, joining an existing practice is a strategic option. This is mainly because access to an active revenue stream, insurance credentials, and a robust client base is immediate. Another advantage of joining an existing practice is that you don’t have to put limited funds toward marketing, nor do you need business experience.
Culture
A trusting patient relationship needs a positive work culture to thrive. “Positive work culture will always support the healthcare professional-patient relationship. It will build patient trust and gain confidence among staff who provide patient care,” an NIH report concludes. “It will allow them to feel that other than the goal of working to cure their diseases, they receive care.”
The NIH study found that when patients see doctors and nurses who are satisfied in doing their work and providing services, it encourages patients to follow instructions. “When they feel teamwork is active among staff and stable leadership exists from their managers, these patients may be more than willing to allow themselves to seek medical advice and treatment.”
The advantages of joining an existing dermatology group practice have a considerable impact on your success. But the ease of stepping into an established practice can also interfere with the long-term benefits. For instance, joining an established practice means someone else decides who you will treat, the billing software you will use, and the length of your appointments.
By comparison, when you open your practice—and on the condition that your financing is secure—you have more control over your patient volume. You’re also in charge of your office hours, appointment times, services, billing, and lab partnerships.
In a group practice, the bottom line is the main focus. It’s part of the motivation to maintain a fast pace and see as many patients as possible. It can also mean a lower pay rate for you. It’s no wonder almost half (42 percent) of physicians experience burnout. And that’s something to be mindful of when making long-term business decisions.
Customer
It’s important to establish the type of patient care you want to offer. Those decisions can help you prioritize resources, possible clinic locations, and equipment purchases. For example, does your area report high incidences of skin cancers? How many dermatology clinics presently specialize in the services you hope to promote? One phone call can help you establish the wait time for new patients. Addressing these questions can guide your professional goals for your patients. But there are other factors to consider.
Your customer base includes more than your patients: It includes billing partners, insurance companies, lab partnerships, marketing firms, other healthcare providers, and more. When you own your clinic, you get to select and nurture those valued relationships.
Strategic partnerships, such as your dermpath lab, can help streamline your workflow process and reduce overhead costs. For example, working with a lab with expertise in digital pathology means you don’t need to invest in expensive lab and testing equipment. Partnering with a lab that integrates with your EMR technology and offers locum tenens services may open up new opportunities to expand your services without investing in an expanded staff.
By working with innovative, digital-based companies like PathologyWatch, it’s easier to see the possibilities of opening your own practice.
The healthcare industry will show plenty of opportunities for dermatology services in 2022. Choosing the best way to promote your expertise with optimal patient care can be a rewarding next step in your career. Improve your chances of long-term success by weighing the pros and cons of a group practice versus starting your own dermatology clinic (your financial strength, work culture, and customer relationships) and chart your new path forward.
Nov 18, 2021 | Dermatology Practice
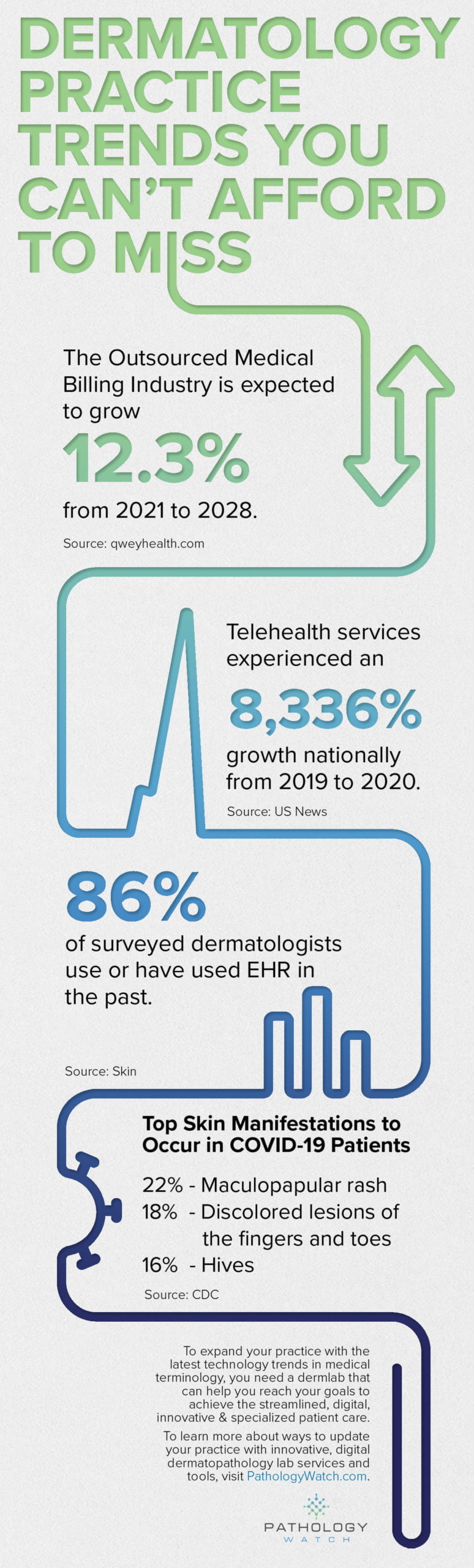
In some ways, it took a pandemic for the healthcare industry to accelerate new ways to deliver patient care. For example, a CDC study found that using telehealth for patient visits increased by up to 154 percent from 2019 to 2020. Now, this service is a permanent option for some major healthcare organizations, and it’s just one example of how dermatological interoperability is helping providers to move closer to incorporating technology with traditional patient care.
A recent study determined that effective interoperability and communication are essential for a primary care system to successfully prevent illness, manage care across multiple providers, and reduce health care costs.
“To address patients’ needs, primary care physicians often must communicate and exchange information with specialists, hospitals and other care settings, social service providers—and, of course, the patients themselves,” says Muhammad Chebli of NextGen Healthcare.
But what is dermatological interoperability? If it’s the future of healthcare, how can we incorporate this technology in ways that help your practice run more efficiently and grow? Let’s first gain a better understanding of interoperability. Then, we’ll explore how interoperability can scale our practice with innovation that better organizes data, expands patient care options, and streamlines billing.
What Is Interoperability?
For doctors who have already adopted EMR technology, you are closer than you think to full interoperability. “EMR interoperability is a system architecture that allows healthcare facilities to access, analyze, and share health data between systems, medical devices, and applications at a local or cross-organizational level,” explains Ivan Dunskiey, Demigos Healthcare founder and CEO.
Almost 90 percent of healthcare providers have implemented EMR technology into their workflow processes. As dermatologists work with EMR technology, here are six ways EMR can work for them.
1. Ensures Compliance
Under the federal government’s direction, the healthcare industry is placing patients at the center of their care and medical information. Part of the 21st Century Cures Act entitles all patients to access their complete medical file upon request.
In other words, providers must digitize their patient records so that patients can access their information. As patients take a more active role in their care, doctors can use these opportunities to develop open, trusting patient relationships.
2. Standardizes Data
Is it a rash? Psoriasis? A lesion?
It’s not uncommon for patients to be treated by more than one doctor at a time. With hard-copy record keeping, a healthcare provider may use different terms to describe the same thing. Using EMR interoperability standardizes those terms, which creates more accurate, reliable patient data.
Also, with standardized data, other health service agencies can collect and analyze data about a specific skin condition, for instance, and note higher incidences of that particular disease in specific geographic regions. That, in turn, can launch discussions on the risks and determine if an area needs more resources.
3. Expands Access to Services
Telehealth services and self-service patient portals are promising indicators of the evolution of care delivery options with interoperability. For the dermatology field, EMR and digital slides sometimes open up life-saving treatment options for malignancy cases. Regardless of clinic size and location, doctors can obtain expert opinions on dermatology cases and discuss results via remote.
4. Allows Access to a Complete Patient Medical Record
The more information a healthcare provider has, the better the diagnosis. Since patients only remember about 49 percent of the information they receive from their doctors, medical professionals must rely on thorough medical records. With digitized patient records, a healthcare provider not only sees their notes, but they can also read through the notes shared by other doctors.
When determining treatment options, a healthcare provider can refer to reported lifestyle habits or existing conditions being treated by another physician that could interfere with certain treatment plans. Accessing a complete patient record ensures effective care that won’t interfere with other treatments, medications, etc.
5. Faster Billing
There are several reasons why digital patient records streamline the billing process. “Technology has enabled a huge transition in streamlining medical records storage and processing,” explains Greg Dondero, business development director at Healthcare Resource Group, Inc. “Electronic recordkeeping helps ensure that patient data is accurate, up to date, and easily accessible. It allows secure sharing of information with patients, providers and other healthcare workers, which ultimately reduces costs because of reduced manual paperwork.”
6. Saves Time
At this very moment, a collective “hah!” resounds from doctors who recently implemented a new EMR system. In fact, one of the most common complaints among doctors is how much time it takes to update patient records. One study estimates that surgeons, for example, spend almost two hours per day updating electronic health records. And they often update patient files at home in their spare time.
As EMR technology evolves (and it will, as more doctors weigh in with feedback), so should your workflow design. For example, how do you handle patient check-ins? Can the patient verify insurance and contact information through a self-service portal before their appointment? Are there redundant tasks within your office workflow that can be automated? Can you schedule time each day for communication tasks or file updates? Partnering with a full-service digital dermpath lab like PathologyWatch can fast track your workflow WITH technology to help you save time and make it easier to scale your practice in conjunction with these innovations.
No doubt about it: Interoperability is the future of EHR and EMR systems. A better understanding of the possibilities dermatological interoperability can bring to your patient care, billing, and data management is transformative for the future of your practice.
Sep 22, 2021 | Dermatology Practice, Digital Pathology, Pathology Business
The Texas Dermatological Society (TDS) is getting ready to roll out the red carpet—Texas-style—for their 2021 Annual Fall Meeting.
In preparation for this event, we sat down with Laura Madole, executive director at the TDS, to talk about the upcoming 2021 Annual Fall Meeting to be held virtually on September 24–25, 2021. In the past, the in-person TDS event welcomed almost 400 attendees to their annual spring and fall meetings. This time, TDS looks forward to hosting hundreds in a virtual setting.
Despite the changes prompted by COVID-19, which forced TDS to cancel their spring 2020 event, Laura is confident that attendees, sponsors, and exhibitors will enjoy the unique features of this virtual meeting.
“We were a little nervous,” admits Laura, concerning their switch to virtual meetings. “So while we hope we can open doors in the spring of 2022, the virtual event has been the next-best option.” In fact, the fall 2020 and spring 2021 TDS events attracted almost 500 attendees.
The unexpected benefits of hosting a virtual event focus mainly on the accessibility of the event. “It opened up opportunities for us to connect with members living in rural areas or other members who are residents at Texas Tech, for example, who can’t easily get to these events,” she says.
Experience a Unique, Interactive Virtual Event
TDS is using a company called vFairs, which invites attendees to visit customizable virtual exhibit halls, rooms, and vendor booths. Attendees can reach out directly to exhibitors and sponsors via video chat or direct text messaging. Plus, all of the attendees are listed, so face-to-face chat is easy.
Laura says that many of these attendees have known each other for years; it’s a fun and fantastic way to earn CME credits. But if this is a member’s first time attending the event, she has some tips for a successful virtual experience.
“I recommend just going in and looking around within the platform: click around and get familiar with the layout. There’s an auditorium, a virtual lobby, a lounge, and several other rooms. I’d definitely utilize the chat feature at a meeting, so it feels like you’re surrounded by your friends and colleagues. It’s more fun when people can interact on the platform.”
The virtual element definitely encourages participation among residents who often have difficulty attending in-person events. Laura says that TDS usually hosts around seven podium presenters for the resident competition. But with virtual, they are delighted to offer 19 podium presenters this fall.
Take Exhibitor Information with You
This is not a typical Zoom meeting. The vFairs platform provides a hotel lobby feel that engulfs attendees in a rich, virtual world filled with uniquely designed exhibits and booths. Guests can virtually stroll amid custom-designed booths, or they can move directly to a booth of their choice from a directory.
“While we enjoy meeting people face to face at events like this, virtually connecting with people who are genuinely interested in learning more about our technology is a fantastic opportunity,” says Rachel Reeg, senior sales director at PathologyWatch. “At in-person events, you compete with high-volume activity that can be distracting, and people often limit the time they spend at your booth. With the virtual briefcase, we can provide valuable information through video, downloadable case studies, ebooks, product information, and other resources that guests can look through when it’s convenient for them and reach out if they want to know more.”
After the conference, attendees will receive all of the information they saved in their virtual briefcase via email. This is a great feature for attendees to keep track of exhibitor information without the risk of losing papers or accidentally leaving them behind. Since the materials are digital, exhibitors can promote products and services through expanded forms of media; a feature that isn’t possible at in-person events.
Host a Social Scene, Just on a Screen
For Laura, the conference is an ideal opportunity to interact with members. “There are many components of my job with the TDS. There are meetings, but there are also membership duties. There’s a financial side and boardwork, and grants, and grant-writing,” she says. “With all of those duties, it’s always a good refresher to be surrounded by our members and make personal connections. That interaction reminds me why I do the job that I do. I love it. I do it for my members, and I hope these meetings are a benefit to them.”
The event offers attendees required CME credits as well as the one-hour ethics credit required for those practicing in Texas. But the platform also hosts a background gamification. A visit to the leaderboard shows attendees how to accumulate points from participating in sessions, visiting exhibit booths, and more.
“For those who are present, and based on the leaderboard points, I will be doing raffles throughout the conference,” says Laura, who promises some amazing prizes for the winners.
Although hosting virtual events may be a temporary condition for TDS, Laura is partial to the idea of maintaining a virtual component to future events. “I would love to offer a virtual component to our events because it’s a member benefit,” she says. “Members being able to attend from anywhere in Texas if they can’t attend a physical event is huge.”
She believes that incorporating virtual sessions or activities in conjunction with in-person events is a great offering for members. But the upcoming fall event is the main focus, and it’s shaping up to be “virtually” one of the most engaging, must-attend dermatology events of the season.
For registration and event information, click here.