Images shown are not intended to be used for the diagnosis or treatment of a disease or condition.
Providing your patients with definitive diagnoses requires clear and thorough dermatopathology reports. Many clinics and healthcare groups are permitting patients to log in and view these reports. However, a recent survey indicates patients are nearly three times as likely to misinterpret a dermatopathology report and conclude they have an incorrect diagnosis over the correct diagnosis.
“As patient access to pathologic test result reports increases, it is important to consider best practices to minimize potential negative consequences for patients and clinicians,” notes Hannah Shucard, MS. With patient satisfaction as the number one priority, you want to make sure your reports are complete and easy for everyone to interpret, in addition to meeting the standard of care.
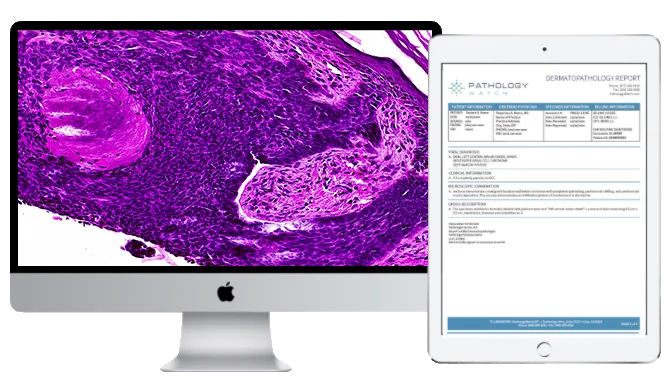
There are several sections in a dermatopathology report. Below, we’ll review the purpose of the final diagnosis, microscopic descriptions, gross descriptions, clinical information, changes and corrections, and compliance to ensure your dermatopathology reports are understandable for you and your patients.
Final Diagnosis
As the most important part of a dermatopathology report, the final diagnosis should designate the results of the disease process seen in the biopsy or tissue. Sometimes, there is a comment section that describes further clinically relevant information, such as margin status, treatment recommendations, or other studies’ results. Diagnoses should be definitive in the vast majority of cases.
Microscopic Description
In this section, we find descriptions of the morphological features of the disease process seen under the microscope. Many pathologists use standardized text descriptions that elaborate on the key features that are unique to that disease. The Microscopic Description also describes the results of stains used to assist in making the diagnosis.
Gross Description
This section describes the size, color, and texture of the tissue that was received in the laboratory. This is an important section that is used by the submitting clinic and provider to ensure that the correct specimen is being examined. The laboratory also describes any inking or cutting that was done to the tissue prior to processing it to make glass slides. Specimen orientation with inking is also included in this section.
Clinical Information/Impression
The Clinical Information provided by the clinic and provider on the pathology order form is some of the most critical data that a laboratory and pathologist can receive to generate an accurate report. The information includes clinical differential diagnosis or clinical history. The Clinical Information section is also used for quality assurance by the dermatologist to ensure that the Final Diagnosis section correlates with clinical findings.
Changes and Corrections
Sometimes, additional clinical information or discussion can lead to a revised report. If the information does not significantly affect the Final Diagnosis, the laboratory will issue an “Addendum,” a secondary report that includes the new information. Rarely, corrections need to be made to a finalized report. In this instance, an “Amendment” report is issued, outlining the corrections that have been made. Common causes for amended reports include correcting the specimen site or demographic information. However, these should be rare occurrences.
Compliance
There are several other components to a laboratory report which are necessary to comply with laboratory licensing standards outlined by CLIA (Clinical Laboratory Improvement Amendments of 1988 (CLIA 493.1291)). These include patient identifiers, the testing laboratory’s location, test report date, and specimen source. A Billing section is sometimes added for auditing purposes.
Dermatology clinics carry an essential responsibility to make sure their patients receive accurate and organized diagnoses. Ensuring that the dermatopathology laboratory provides clear and precise reports that meet the industry standards is crucial to delivering the highest quality of clinical care possible.