By April Larson, MD
Thirteen is shaping up to be a very fortunate number for digital pathologists in 2023. Thanks largely to the efforts of the College of American Pathologists (CAP), the American Medical Association CPT Editorial Board developed 13 new Category III digital pathology digitization procedure codes. The 13 new add-on CPT codes, which have been introduced to record the use of digital pathology, went into effect on January 1.
Prior to 2023, lab reports in the US used the same CPT (current procedural terminology) codes in reporting any diagnostic read—with no distinction made as to whether the diagnosis utilized digital pathology or a glass slide under a microscope. Thus, both procedures earned the same reimbursement rates.
The new CPT codes will help track the additional work and investment of digital pathology into practice and help establish a new standard of care by demonstrating its wider acceptance and usage by the medical community, which in turn is a big step in receiving reimbursement for those services. This will continue to push the medical industry toward the adoption of digital pathology, increasing the availability of remote pathology work for pathologists.
Let’s look at the difference between Category I and the new Category III CPT codes and how they could lead to reimbursement rates for those practices utilizing digital pathology.
The Difference Between CPT Codes
The 13 new Category III codes are designed to be temporary in nature. They’re intended for emerging technology, services, and procedures and allow for the data collection directly associated with carrying them out. The goal is to show that these procedures are becoming more commonly adopted so that pathologists can then work with the AMA to shift these codes to Category I status.
I believe the use of these new CPT codes is a helpful measure that the government can use to determine whether new technology—in this case, digital pathology and the use of AI prognostics— is actually advancing the standard of care.
How do Category III codes differ from Category I codes? According to CAP, the new Category III codes may not meet one or more of the following Category I requirements:
- All devices and drugs necessary for the performance of the procedure or service have received FDA clearance or approval when such is required for the performance of the procedure or service.
- The procedure or service is performed by many physicians or other qualified health care professionals across the United States.
- The procedure or service is performed with a frequency consistent with the intended clinical use (e.g., a service for a common condition should have high volume, whereas a service commonly performed for a rare condition may have low volume).
- The procedure or service is consistent with current medical practice.
- The clinical efficacy of the procedure or service is documented in literature that meets the requirements set forth in the CPT code change application.
Category III codes should be reported only for primary diagnostic use; they should not be reported if the digitization performed is solely for archival or educational purposes, developing a database for training or validation of AI algorithms, or for conference presentations.
The 13 new codes are attached to different services and procedures, but the one thing they all have in common is involving the digitization of glass slides.
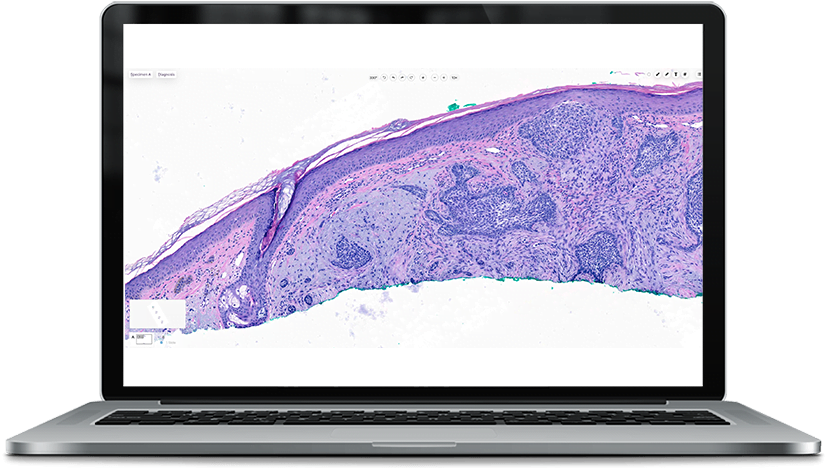
The use of these codes is exciting both for dermatologists and dermatopathologists. What we’ve seen at PathologyWatch is that dermatopathologists can benefit from remote digital workflows, and dermatologists have quicker access to both digital slides and reports.
Reclassification to Category I codes, which is the goal, requires meeting both general and specific criteria as determined by the AMA.
Potential Game-Changer for Pathologists
While temporary in nature, the 13 new codes have the potential to be revolutionary for digital pathologists for a variety of reasons. Of primary merit is that the codes are widely expected to achieve Category I status in the near future, opening the door to new financial reimbursements.
Clearly, there are significant upfront expenses associated with digital pathology. The initial technology investment, for example, can seem formidable, with scanners running anywhere from $250,000 to $1 million.
While it is important to note that there are presently no reimbursements directly tied to the new CPT III codes, the change is laying the groundwork by bringing a different dynamic into play.
The utilization of CPT codes helps establish the frequency of usage within the medical community. In order to determine reimbursement, this is often determined by committees of experts who help document the financial investment required to use a new technology.
Much like radiology, the wide adoption of digital pathology will help improve the quality of patient care by promoting sharing of information and images with consulting providers, which improves communication and coordination of care. It also promotes more frequent peer-to-peer and expert consultation with difficult cases and patient education and understanding of their disease.
Reimbursement also provides a financial incentive for clinics and labs to invest further in digital pathology. CAP proposals are being considered for development in the next few years through the AMA CPT process. In the meantime, it is important for dermatologists and dermatopathologists to use the new Category III codes to properly track their digital pathology services.
View a chart with the new CPT codes and detailed explanations of what they entail at cap.org. Then, contact us to learn more about how these new codes, and the adoption of digital pathology, could greatly improve your level of patient care and your practice in general.
— April Larson, MD, is chief medical officer and a cofounder at PathologyWatch.