Mar 8, 2023 | Pathology Business
Slice of Healthcare honors PathologyWatch CEO for innovative and influential leadership in digital health space.
SALT LAKE CITY (PRWEB) MARCH 07, 2023
Dan Lambert, CEO and cofounder of PathologyWatch, a full-service digital dermatopathology solution, was named one of the Top 35 Digital Health Leaders by Slice of Life Healthcare in its first annual list celebrating the most innovative and influential leaders in the digital health industry.
Slice of Healthcare is a top healthcare media company that produces and manages over 15 podcast shows featuring pivotal healthcare leaders as guests. Fundamental factors considered in selecting the top 35 honorees include their impact on the industry, outsider conversations, funding, partnerships signed, customers signed, experience, role and whether or not they exhibit the ever-elusive “it” factor.
“I am thrilled to be selected for this honor, but even more importantly, I’m excited for the recognition it brings to our mission at PathologyWatch,” said Lambert, who cofounded PathologyWatch in 2017. “Our goal is to bring truly life-saving technology to billions of people who might otherwise never have access to this level of healthcare. We have become excellent at one field of pathology by staying very focused on the study of skin cancer. The current and future capabilities of our single-solution system are very exciting, and we’re appreciative to be recognized by Slice of Healthcare.”
After receiving a degree from BYU in computer engineering, Lambert earned his MBA from Harvard Business School. A former executive at IBM, he has led multiple successful ventures and company exits to private equity. In 2018, Lambert was named an Inc 500 CEO for his work on BoardVitals, a medical education company.
“At PathologyWatch, Dan’s leadership style enables us to stay very focused on what we need to be doing to fulfill our mission,” says Michael Torno, Chief Revenue Officer. “It’s easy in a startup to go down all sorts of avenues and try to address everything all at once, because you see so many possibilities. What Dan does as a leader is keep us very engaged in doing something very, very well. It’s just crazy what he’s doing, and what he’s already done and accomplished. This latest recognition is well earned.”
The Slice of Healthcare Top 35 Digital Health Leaders list was compiled after an extensive internal and external research process that spanned more than six months. The final list showcases some of the industry’s most accomplished leaders in the digital health realm. Honorees include Chief Executive Officers, Chief Medical Officers, serial entrepreneurs, first-time founders and seasoned leaders.
“We are super excited to announce our first annual Top 35 Digital Health Leaders list,” said Jared S. Taylor, founder of Slice of Healthcare. “These leaders are making strides in digital health and adjacent areas, which is no easy task. We are proud to recognize their contributions and to bring attention to their innovative work.”
For more information about Slice of Healthcare and the 2023 Top 35 Digital Health Leaders, please visit sliceofhealthcare.com. For more information about PathologyWatch, visit pathologywatch.com.
About PathologyWatch
PathologyWatch is the groundbreaking leader of digital dermatopathology services. Through these services, dermatology clinics, hospitals and laboratories can improve operational efficiency by speeding up workflow and enhancing patient outcomes by utilizing the PathologyWatch expert professional team and laboratory services. This can facilitate best-in-class reads and, in some cases, enable additional revenue to the practice by in-housing pathology. With an intuitive and easy-to-implement digital pathology solution that includes access to top-tier dermatopathologists and a streamlined clinical workflow that interfaces directly into the EMR, PathologyWatch brilliantly combines state-of-the-art technology and clinical decision-making to deliver unprecedented patient care.
Feb 7, 2023 | Digital Pathology
As the global demand for dermatology solutions has increased, PathologyWatch has been at the forefront of serving both patients and clinicians through innovation in digital dermatopathology. By providing benefits like increased efficiency, enhanced patient care, and new opportunities for revenue growth, PathologyWatch is recognized for transforming the dermatological experience for providers and patients alike.MedHealth Outlook recently ranked PathologyWatch as one of the top 10 dermatology solution providers across the globe. In its feature, CEO Dan Lambert shares how PathologyWatch is helping reduce the cost of pathology while creating better patient care across the country. Read on for key highlights, or visit this link to read the full article.
The Need for Digital Transformation
Simplifying the clinical workflow results in optimal clinical decision making and enhanced patient care. Without a computerized pathology platform, hospitals and dermatology clinics miss out on increased efficiency by sharing digital histologic slides and direct interaction with the preferred EMR.
PathologyWatch provides this increased level of care and efficiency not only through its digital tools but also its network of academic-level dermatopathologists and expert consultation. With around-the-clock access to knowledgeable telepathologists, hospitals and clinics can rely on PathologyWatch for expert locum tenens support at any time. By saving both time and money with PathologyWatch, healthcare providers can better position themselves for whatever the future may hold.
How Do Digital Pathology Services Work?
By combining the knowledge and technology of an academic center with the efficiency and customer service of a private lab, PathologyWatch helps labs embrace digital transformations quickly and keep everything functioning efficiently. Within just three to six months, PathologyWatch and its team of experts can help clinics complete this transition and manage digital pathology diagnostics in a wide variety of subspecialties.
To continue helping patients receive faster diagnoses and equal access to dermatopathology services while empowering laboratories, PathologyWatch is pursuing expanding its reach with artificial intelligence. This tool will provide even more value to PathologyWatch’s services, which already include completely integrated EMR reporting and round-the-clock access to digital slides. Thanks to PathologyWatch’s end-to-end solution, dermatologists now have access to an effective integration of EMRs, laboratory information systems, scanners, and digital viewer technologies.
PathologyWatch in Action
PathologyWatch’s partners that digitize consistently report a net positive return on investment. When facing challenges related to understaffing, overflow volume, or difficulty managing rural operations, providers turn to PathologyWatch for help.
Cedars-Sinai Medical Center is a classic example of how PathologyWatch provides value to its clients: Wanting to grow its outreach, Cedars-Sinai partnered with PathologyWatch for novel growth solutions in a new demographic, access to experts, and broad insurance coverage.
However, Cedars-Sinai isn’t the only clinic that has been transformed by PathologyWatch. “We are honored that of all the digital dermpath labs available, dermatologists are increasingly choosing to partner with us,” says Lambert. ”As digital dermatopathology begins to grow, it has the potential to reduce the costs of pathology by billions while creating better patient care for everyone across the country. We’re thrilled to be winning so much volume so quickly.”
To read the full article, click here.
Jan 11, 2023 | Dermatopathology Lab
Pathologywatch Implements AI Technology That Detects 5 Skin Lesion Types with Higher Sensitivity than Previously Published AI Model
Authors: James Requa, Tuatini Godard, Rajni Mandal, Bonnie Balzer, Darren Whittemore, Eva George, Frenalyn Barcelona, Chalette Lambert, Jonathan Lee, Allison Lambert, April Larson, Gregory Osmond
Highlights
- Including a large dataset of hand-drawn annotations increases the sensitivity of AI.
- Integrated supervised and semisupervised learning is superior to other AI models.
- Multilevel training permits subtyping, localization, and margin detection.
- Dermpath involvement in model development can ultimately improve model performance.
- Increased confidence in AI-assisted diagnoses can lead to improved patient care.
Abstract
Background
Skin cancer is the most common malignancy diagnosed worldwide, accounting for over 30% of all cancer diagnoses. Equally troublesome is the 77% increase in nonmelanoma skin cancers over the last several decades and a 250% increase in melanoma cases in children, adolescents, and young adults since 1973.
Objective
The goal of this study was to create an AI model that detects and classifies skin lesions with a higher degree of sensitivity than previously demonstrated. This AI model (i.e., Mihm) has the potential to match and eventually surpass expert pathologists and improve clinical workflows.
Methods
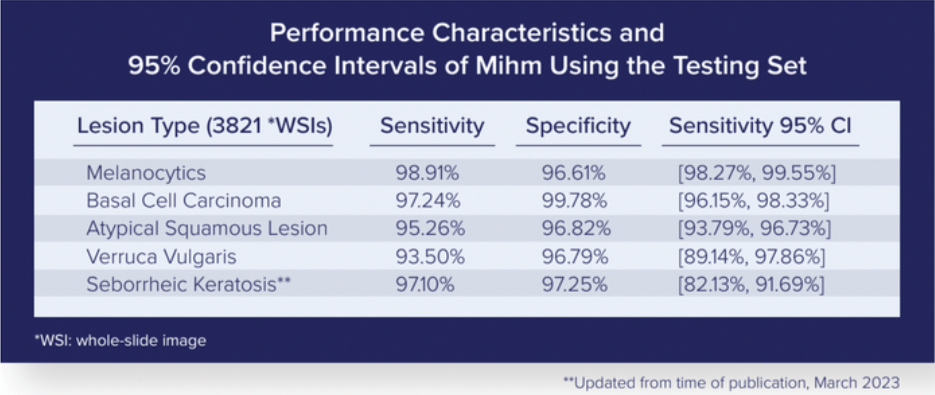
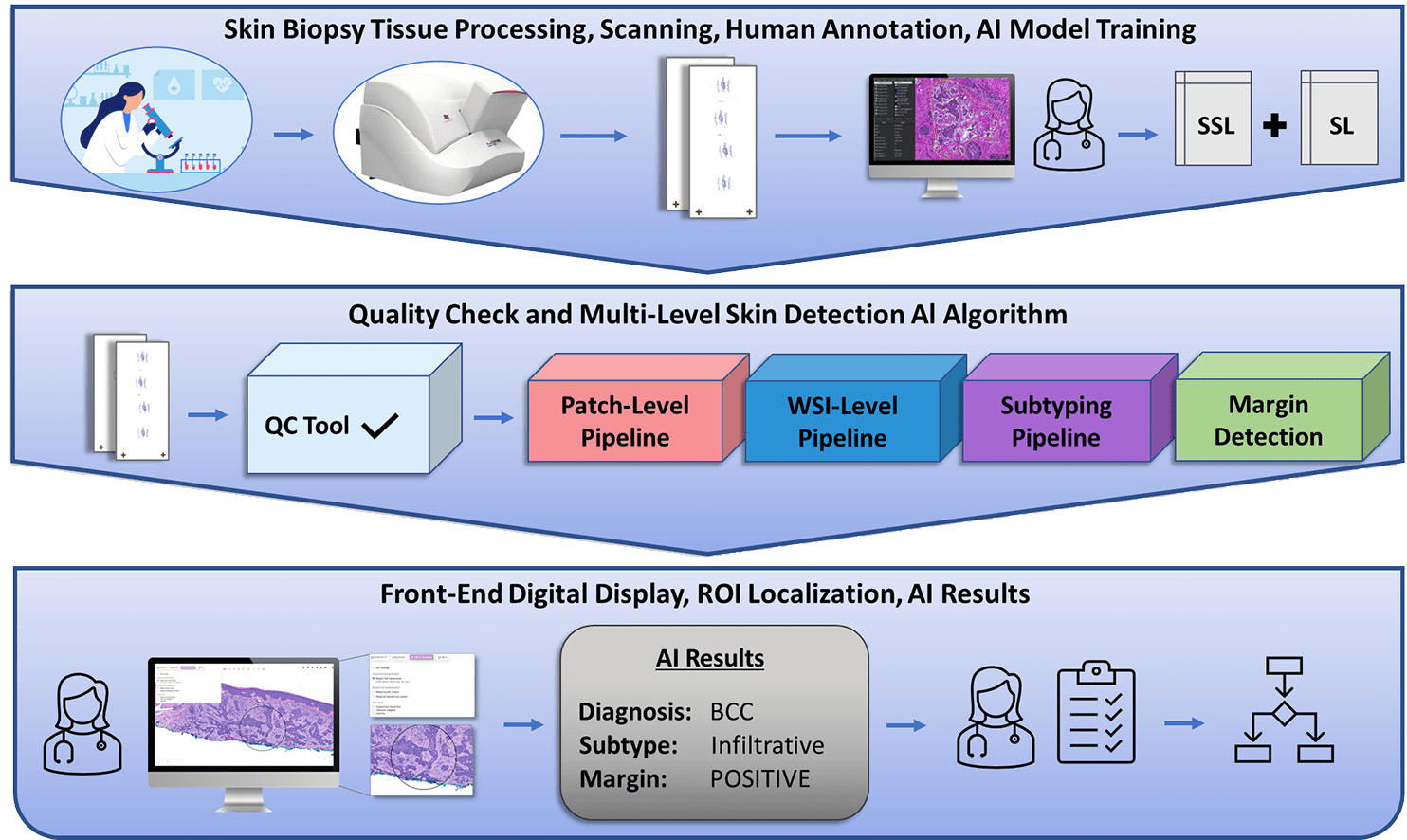
We produced an end-to-end multilevel skin detection system by combining supervised learning (SL) with semisupervised learning (SSL). This system detects five main types of skin lesions with high sensitivity and specificity. In addition, it detects subtypes while also localizing and providing margin status to evaluate the proximity of the lesion to nonepidermal margins.
Supervised Training Subset
- 2,188 random WSIs collected by PathologyWatch laboratory between 2013 and 2018
- Weekly supervised subset consisting of 5,161 WSIs from daily case specimens
Validation Set
- 250 curated daily case WSIs from PathologyWatch’s tissue archives
- Included 50 “mimickers”
Testing Set
- Composed of noncurated daily case specimens collected from PathologyWatch labs between July 20, 2021, and August 20, 2021
Results
By running the testing set through the Mihm Evaluation Pipeline, we could assess the performance characteristics of our AI model.
Our multilevel detection algorithm (patch-level, ROI-level, WSI-level) can subtype lesions with an AI overlay in the front-end digital display that localizes diagnostic ROIs and reports on margin status by detecting overlap between lesions and nonepidermal tissue margins.
Conclusion
This AI model, which is the result of collaboration among a team of dermatopathologists, detects five skin lesion types with higher sensitivity than previous AI models. It also provides end users with valuable insights in subtyping, localization, and margin status in a front-end digital display.
This end-to-end system can improve pathology workflows by doing the following:
- Increasing diagnostic accuracy
- Expediting the course of patient care
- Improving patient outcomes
Nov 18, 2022 | Digital Dermatopathology, Meet The Team
A noted dermatopathologist, Dr. Willman joins the PathologyWatch team to continue delivering the highest-quality care to patients.
PathologyWatch, a full-service digital dermatopathology solution, welcomes Dr. Joseph Willman, MD, to its team of respected pathologists. Dr. Willman, a dermatopathologist with over two decades of experience, will utilize state-of-the-art digital pathology workflows to deliver optimal patient care to dermatology clinics.
A board-certified pathologist and dermatopathologist, Dr. Willman completed his residency at the University of Utah, his dermatopathology fellowship at the University of Colorado, and his molecular genetic pathology fellowship at the University of Michigan.
Dr. Willman’s connection to pathology began long before his career and training. His father was a pathologist, introducing him to the profession at a young age. Still, he expected to follow a different career path. As a student, he spent time working in emergency rooms and found surgery and internal medicine interesting. However, his third-year medical school pathology rotation cemented his interest in pathology, and he now sees digital pathology as the future of the field.
“I think the majority of anatomic pathology will be done digitally, as technology advances to digitize the slides, because it makes it so easy to collaborate, get opinions on cases and implement quality measures to get multiple people reviewing a single case,” Dr. Willman said. “It’s so much more convenient than shipping or using a courier to share glass slides, which is easily a 48-hour process by itself. PathologyWatch can secure expert opinions from people all over the country in a single afternoon, and that’s revolutionary.”
With 20 years of experience in dermatopathology, Dr. Willman brings extensive expertise to PathologyWatch. Most recently, he served as the director of a national reference laboratory and molecular diagnostics lab, where he worked extensively with quality systems and compliance and regulation. His experience and interest in lab operations will help as PathologyWatch builds a digital laboratory platform incorporating quality measures that aren’t possible in a physical laboratory.
“We are thrilled to have Dr. Willman joining our team, not just for the years of experience he has but also for his enthusiasm for the future and commitment to progress and innovation,” said Dan Lambert, CEO at PathologyWatch. “He will be of particular help in moving our molecular efforts forward.”
Oct 25, 2022 | Digital Pathology, Uncategorized
The digital pathology industry is expected to grow from $736 million in 2021 to $1.37 billion by 2026. PathologyWatch is emerging as an industry leader, blazing a trail for patient care like no other.
In a MedTech Strategist feature, CEO Dan Lambert describes PathologyWatch’s unique position in the dermatopathology space, its success in building a workflow from start to finish, and its unprecedented opportunity to transform the future. Read a few highlights here, or visit this link for the full article.
What Makes PathologyWatch Unique
There are 25 million skin biopsies performed in the US each year and, while many are benign, it is estimated that there will be 99,780 new melanoma diagnoses in 2022. Melanoma is a serious form of cancer that, if left untreated, can metastasize and quickly become fatal. The world is in dire need of a reliable and efficient solution to diagnose skin cancer.
With its focus on dermatology and cutting-edge tools, PathologyWatch is in a unique position to address this critical issue. Unlike other digital pathology companies, PathologyWatch works mostly with outpatient clinics rather than hospitals. This means that PathologyWatch is involved throughout the entirety of the testing and diagnosis process.
Building a Digital Pathology Workflow from Start to Finish
PathologyWatch’s clients asked for more than just a “piecemeal” solution—they wanted involvement at every point in the process. According to Lambert, “They wanted us to manage the transportation of the tissue sample, the courier system, the insurance billing, enhanced bidirectional interfacing, and everything in between.” This was a challenge since they “had to integrate a lot of systems that didn’t talk to each other.”
Lambert adds, “The firm had to build the laboratories, develop a laboratory information system to specifically track skin specimens, buy scanners, create a digital platform usable anywhere (not just in the laboratory setting), forge agreements with payors and partners, and connect with all the major electronic medical record providers in dermatology.”
PathologyWatch was able to successfully build a workflow integrating all the pieces from start to finish. The system integrates with the electronic medical records of Modernizing Medicine, EZDERM, and eClinicalWorks, which cover app. 90 percent of dermatology practices, and the company receives samples from over 120 dermatology clinics, with near perfect client retention.
The Advantage of Control
This fully-integrated system has granted PathologyWatch the control necessary to get accurate, detailed results. “In our own environment, we can assure the quality and standardization of the techniques used to generate a digital image. This means better outcomes for AI. You can get amazing sensitivity and specificity when you take the right algorithmic approach while simultaneously operating in controlled laboratory conditions,” says Lambert.
To read the full article, click here.