Dermatopathologist Eva Vertes George Joins PathologyWatch Team
Dr. George brings years of dermatopathology experience to the firm, with a special focus on melanoma.
Salt Lake City, November 4, 2021—PathologyWatch, a full-service digital pathology service, is pleased to welcome Dr. Eva Vertes George, MD, to its clinical team. A highly qualified and respected dermatopathologist, Dr. George’s expertise in melanoma, autoimmune conditions and inflammatory skin conditions aligns with PathologyWatch’s goals to support the most comprehensive and best-quality patient care while reducing healthcare costs.
“We are impressed with the enthusiasm and depth of expertise that Dr. George brings to the people of Florida and all over the United States,” says Dan Lambert, cofounder and chief executive officer of PathologyWatch.
Dr. George completed her residency in anatomic and clinical pathology at the University of Florida. Her fellowship was in dermatopathology at the University of Florida, and she is US-board certified in anatomic and clinical pathology and dermatopathology.
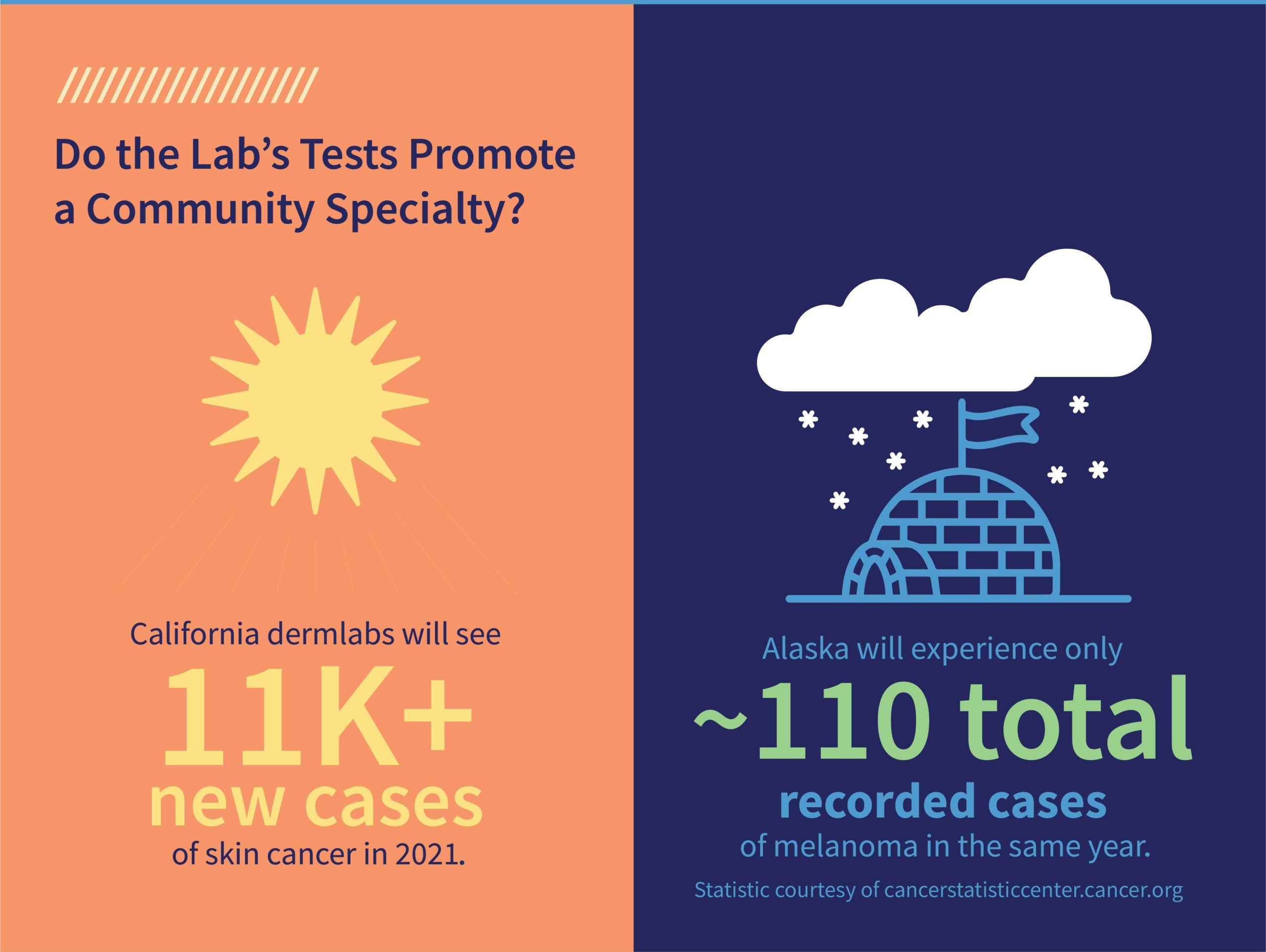
Although she enjoys all aspects of clinical pathology, her focus is melanoma. “I love it all, but I would say the part that grabs me is melanoma. There’s still so much that we don’t know about them. As we continue understanding the different variants, it’s about making sure we get the correct diagnosis so that patients receive the best care possible.”
As a strong supporter of digital pathology, Dr. George was drawn to PathologyWatch in part because of its commitment to opening up access to qualified patient care to the international community. “The idea that a biopsy can be done anywhere in the world, digitized, and then read by a pathologist from a different place in the world is very exciting. The possibilities are endless with that kind of instant accessibility,” said Dr. George.
“One of the most valuable parts of digital pathology is that it is going to enhance the accuracy of the diagnosis in a timely manner. It enables the transfer of information more readily and then extends that service to rural areas,” said Dr. George. “I truly believe digital pathology is the future.”
For more information, please email [email protected] or visit us at pathologywatch.com.
About PathologyWatch
PathologyWatch is the groundbreaking leader of digital dermatopathology services. Through these services, dermatology clinics, hospitals and laboratories can improve operational efficiency by speeding up workflow and enhancing patient outcomes by utilizing the PathologyWatch expert professional team and laboratory services. This can facilitate best-in-class reads and, in some cases, enable additional revenue to the practice by in-housing pathology. With an intuitive and easy-to-implement digital pathology solution that includes access to top-tier dermatopathologists and a streamlined clinical workflow that interfaces directly into the EMR, PathologyWatch brilliantly combines state-of-the-art technology and clinical decision-making to deliver unprecedented patient care.